Surgeries of all kinds have become more and more powerfully assisted by technology, but in most cases it’s still a human holding the scalpel — especially for delicate and complex operations like spinal surgery. Proprio’s technology reinvents the way surgeons see, understand and influence the contours of bone and tissue, improving outcomes and potentially saving lives.
This isn’t a compact X-ray machine or a cheaper MRI. It’s a live aid to a surgery in which precision and accurate, up-to-date information about the patient is crucial. The promise of the technology has also attracted investment: the company today announced $43 million in new funding.
Spinal deformation happens when a condition, trauma or habit causes the natural curvature of the spine to assume outsized or distorted proportions. The most frequent cause is probably scoliosis, which progressively warps the spine and if left untreated can lead to serious disability. To combat this, the spine is fitted with a custom metal frame, attached with screws, that restricts and corrects this tendency, shepherding the vertebrae into a more healthy arrangement.
It’s not unlike getting braces — if teeth were sealed inside the body and there was a millimeter’s breadth between curing and paralyzing the patient. Spinal corrective surgery is commonplace (about 1.6 million of this type are performed yearly) and effective, but it’s also incredibly difficult and specialized work.
And while new tools have emerged over the years to make it safer and more likely to succeed, a given procedure may still require a dozen X-rays and other scans, and the methods of virtually augmenting surgeons’ own senses are stuck in the past.
An example of a scoliotic spine before and after corrective surgery. Image Credits: Proprio
Detailed interior imagery is needed for prep, but by the time they’re in the operating room, the images they have of the patient may be days or weeks old, and for acute conditions or trauma especially this is a huge problem. If the imagery doesn’t match reality, not only could something have happened in the patient’s body, but there’s an increased risk of harm working with outdated info.
If the surgeon senses that the situation may have changed, the patient must be put inside an imaging machine and everyone must clear the room. Imagine doing that mid-surgery, with all that entails! Not only is it disruptive to the procedure and time-consuming, it leads to multiple radiation doses for the patient and the surgeon, who is repeatedly exposed to this process.
From guessing to seeing

A surgeon conducts an operation with a Proprio Paradigm device overhead. Image Credits: Proprio
Proprio is a startup that aims to completely change how this and other procedures are accomplished by, mapping detailed pre-operative scans to a real-time 3D representation of the patient’s anatomy, running through a complex suite of sensors that monitor movements and changes at a sub-millimeter level.
The company’s first product, Paradigm, is a real-time surgery guidance device comprising a complex multi-camera imager and a display that shows exactly what a surgeon needs to know in order to drive a screw down the exact trajectory necessary to attach the brace without splitting the vertebra or piercing the spinal cord and crippling the patient.
To do this, it performs a hyper-precise version of what your phone might do for an augmented reality app, which tracks the space and objects around you to place a virtual character or piece of furniture in the desired place. Though there are some systems that do something like this already, they rely on combining static, pre-operative imagery with a physical marker as a reference point. Essentially, they don’t track the physiology of the patient, but rather the marker itself, meaning the position of the vertebrae, etc. — a confident guess rather than observed fact.
It also means if the person shifts, or the surgery is delayed, or for any other reason the imagery becomes out of date or misaligned, the systems cease to be effective — remember, being off by even a tiny amount is disastrous; neurosurgery isn’t a discipline where people just eyeball it.
Proprio’s device leapfrogs these methods through very, very precise imaging and computer vision. The “Prism” imaging array has half a dozen sensors in it, including multiple RGB cameras, infrared stereo cameras and a dedicated depth sensor.
I visited the Proprio office in Seattle and saw a live simulated procedure and some development prototypes. CEO and co-founder Gabriel Jones and co-founder Jim Youngquist answered my various questions, though I did not take their answers down verbatim.
Pediatric neurosurgeon, co-founder and Chief Medical Officer Dr. Samuel Browd seemed genuinely excited and relieved by the promise of the tech; obviously it’s his company, but it was clear to me that he considered his first duty to be to his patients, and thought of the Proprio approach as a long-awaited game-changer.
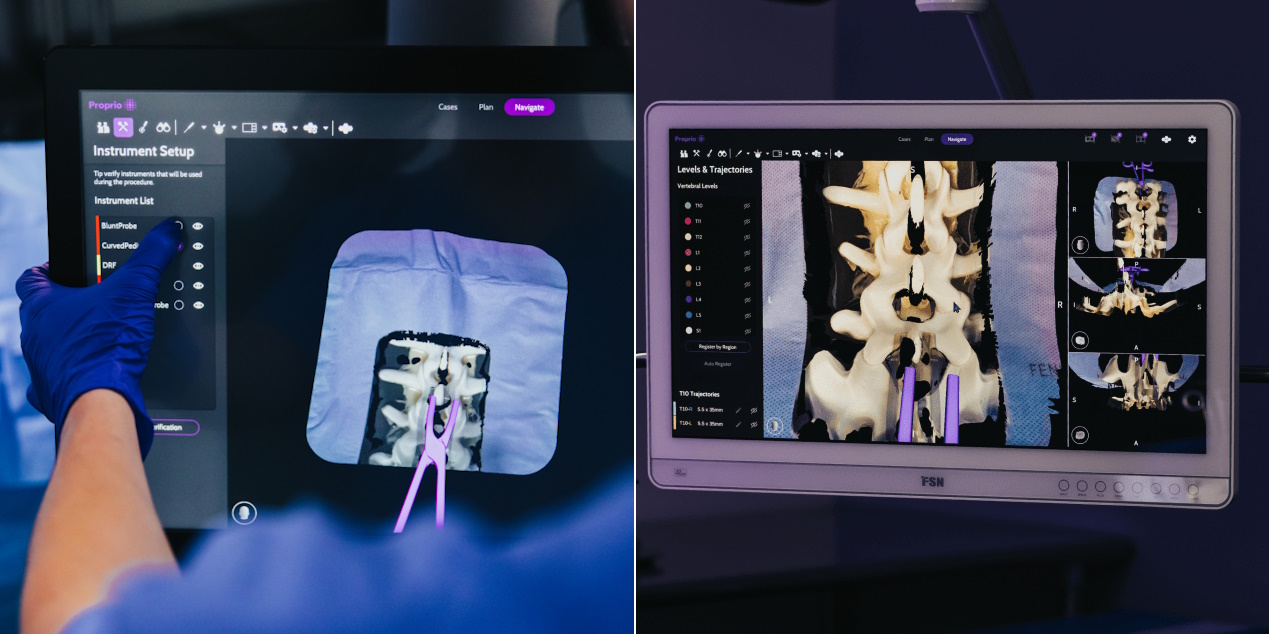
Examples of real-time imagery during a simulated procedure. Image Credits: Proprio
Paradigm also works with pre-operative imagery, but not static images of the positions and orientations of vertebrae. Instead, the vertebra are rendered in 3D as the movable, dynamic objects they are, and the imaging unit can observe and “register” their positions in real time, no marker necessary. (The company’s “light field” talk may ring a bell — and indeed former Lytro engineer Thomas Nonn works on Paradigm.)
So if the patient moves, or needs to be moved, or for whatever reason the vertebrae are not exactly where they were when the MRI was taken… no problem. The system tracks them continuously in 3D space by minutely observing the exposed surfaces and other factors. While accuracy is not an easy metric to track down in such a variable context, the company did say it was at the “sub-millimeter” level.
How this is done is part of the company’s secret sauce — I saw several prototypes from their development process, with different numbers and configurations of cameras. The final design for Paradigm incorporates the best of those and is also, of course, all set up for work in an operating room.
OR and beyond
Proprio in April received 510(k) clearance from the FDA, which is not a full green light exactly, but rather like saying you have an improved version of something already on the market that doesn’t add any new risks. In this case it’s devices for “stereotaxic navigation for spine surgery,” and the company “performed many usability and performance studies with everything from benchtop models to porcine samples and human cadavers.”
Its next step, then, is to commercialize the platform by putting it in as many operating rooms as possible and taking on its first in-human cases. That involves a lot of manufacturing, testing, training and support — few surgical aids are “set it and forget it” type devices. That said, they expect the first procedures to happen this summer at partnering hospitals.

The Proprio Paradigm device, and the door to the company’s “precision lab.” Image Credits: Proprio
But while spinal surgery navigation is the first and clearest application of the technology, it may well only be the company’s opening move. There is, of course, the potential to apply the device’s capabilities to other difficult surgeries — while it was built with spinal procedures in mind, the same method would be helpful in, say, joint reconstruction.
Yet even greater value might emerge from the inevitable “data play,” though surgery is an area where such a play is desperately needed. Training new surgeons is a long and difficult process, and there is a distinct lack of rich data pertaining to any given procedure. There may be video, or not, of varying quality and recency. But high-fidelity collection and analysis of operations is less common than you’d think, and what’s out there is limited in other ways.
The Paradigm imager collects an enormous amount of data, which can be put to use in countless ways (of course all staying well within patient confidentiality laws and ethics). Training is an obvious one, but the team also showed how, by combining data from hundreds of previous surgeries and outcomes with real-time tracking of the patient, a prediction or projection of how a procedure might be improved. It may not be obvious even to an expert eye, but placement of a screw a millimeter over, or tightening a wire by a hair more, could be the difference between requiring a follow-up surgery or not.
There’s also the possibility of tracking the surgeons and tools themselves; if complications occur, for instance, the procedure can be watched start to finish in high fidelity 3D, and the cause of the problems made clear in retrospect. And for the inevitable questions of insurance, malpractice and so on, it could also be used to show clearly that an instrument was used properly, or not used at all, or that it was this person and not that one who made a mistake.
While these capabilities are notional right now (videos I was shown were mockups), they’re certainly possible, but with a device like the Paradigm looking down on every surgery and producing an enormous body of data. While the concept may seem a bit repulsive from outside the OR, Dr. Browd seemed to think it would save many lives and make these procedures faster, better and cheaper.
Data-driven healthcare goes beyond electronic records and telehealth — and even robotic surgeries. There’s room for technology to make many procedures better for both patient and surgeon, if the understandable reticence to part with tried-and-true methods can be overcome.
The company’s $43 million B round came from new and existing investors DCVC, BOLD Capital Partners, Bird B. AG, Cota Capital, Intel and HTC.
Source : A high-tech third eye for neurosurgeons, Proprio could change the OR forever











